Hallux valgus, more commonly known as a bunion, is a progressive deformity of the big toe that is often painful and unsightly. It primarily affects women (4 women for every man) and can appear as early as adolescence or adulthood, worsening over time if no measures are taken to slow its progression. While surgery is an effective solution in painful and/or advanced cases, many people wonder how to prevent hallux valgus before it reaches that stage. Fortunately, it is possible to take preventative action to lessen its effects.

Preventing Hallux Valgus
Preventing hallux valgus involves addressing risk factors, performing specific exercises, and choosing appropriate footwear. The goal is to slow the progression of hallux valgus before it becomes painful and/or makes wearing shoes difficult and/or becomes disabling.
Modifiable Risk Factors for Hallux Valgus
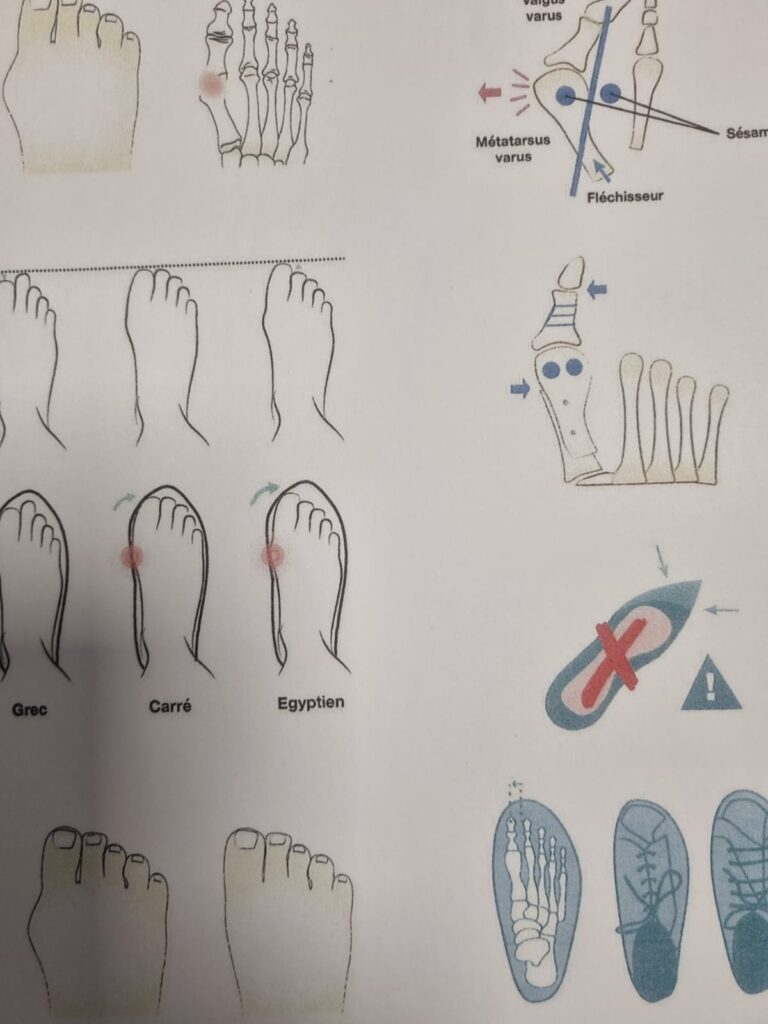
The development of hallux valgus is multifactorial. While certain factors such as heredity or foot shape cannot be changed, other risk factors can be reduced.
Insert here a section from the document called “the deformity”
The first modifiable factor is footwear:
Shoes with narrow, pointed, or overly rigid toe boxes, as well as high heels, encourage the deviation of the big toe. Over time, these mechanical constraints worsen the deformity and lead to joint and plantar pain.
Inappropriate footwear should be avoided.
Excess Weight as an Aggravating Factor
Excess weight places additional pressure on the feet, alters posture, and promotes the collapse of the forefoot. Managing weight through proper diet and physical activity helps relieve this strain.
Lack of Specific Foot Muscle Exercises
Another risk factor is the lack of targeted exercises for the intrinsic foot muscles: weakening of the stabilizing muscles promotes joint instability. By regularly mobilizing the foot, one can maintain its strength and flexibility.
Postural Habits
Certain postural habits (feet turning inward, prolonged standing, poor weight distribution) should also be corrected. Paying attention to the body’s biomechanics helps reduce excessive strain on the forefoot.
Taking action at the first signs of hallux valgus can effectively slow the progression of the deformity. Prevention remains a viable and often beneficial approach, especially for those at risk.
Exercises and Stretches to Prevent Hallux Valgus
Preventive exercises for hallux valgus aim to strengthen the foot muscles, improve the joint mobility of the big toe, and correct biomechanical imbalances.

When included regularly in a routine, these movements can truly slow the progression of hallux valgus and relieve associated pain.
Here are a few simple exercises to do at home:
- Big Toe Stretch: While sitting, gently grasp the big toe and pull it back toward a straight position (without forcing it). Hold for 20 to 30 seconds. Repeat 3 to 5 times a day.
- Strengthening the Short Flexor of the Big Toe: Try picking up a towel or small marbles with your toes to activate the intrinsic muscles of the foot.
- Toe Spreading: While sitting or standing, spread your toes apart and hold the position for a few seconds to improve motor control.
- Plantar Massage with a Ball: Roll a small ball under the arch of your foot to relax the muscles and enhance proprioception.
Practiced regularly (5 to 10 minutes a day), these exercises strengthen the foot’s structure and reduce tension on the metatarsophalangeal joint.
It’s also recommended to walk barefoot on natural surfaces (sand, grass) to stimulate the sensory receptors of the foot and improve overall postural alignment.
Finally, consulting a podiatrist or physical therapist can help you obtain a personalized exercise program suited to your morphology and the stage of the deformity.
Shoes to Choose and Avoid
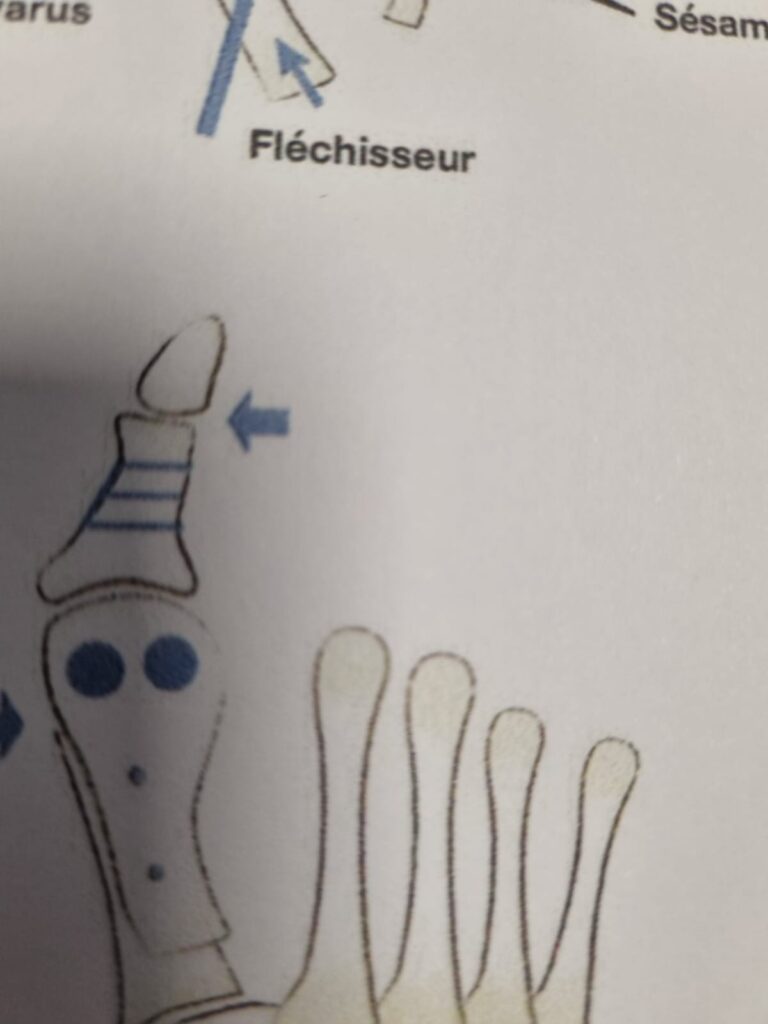
Choosing the right footwear plays a key role in preventing hallux valgus. Poorly designed shoes can worsen the deviation of the big toe, while well-chosen models can help slow its progression and reduce pain. The most expensive shoes are not necessarily the best for preventing deterioration.
To Avoid:
- Pointed shoes: They compress the toes and encourage deviation.
- Rigid and narrow shoes: They prevent natural foot flexion and squeeze the forefoot area. Shoes made from stiff leather are particularly harmful.
- High heels (over 4–5 cm): They shift body weight forward, placing excessive pressure on the big toe joint.
To Prefer:
- Wide, rounded-toe shoes: (Note: In the original French text, it mistakenly says “à bannir” here, which contradicts the point—this has been corrected in the English.) These allow the toes enough space to move freely.
- Consider sizing up: Don’t hesitate to go up one shoe size for better comfort.
- Flexible soles with good cushioning: These help distribute pressure evenly across the foot.
- Arch support: Shoes with good arch support stabilize the foot and reduce strain on the forefoot. Ideally, the shoe should be flexible and wide at the front, semi-rigid in the midfoot and heel area.
- Adjustable models (laces, Velcro): These better accommodate the width of the foot, especially in cases of inflammation.
Try on shoes at the end of the day, when the feet are slightly swollen, to choose a truly comfortable fit.
In more advanced cases, it is recommended to wear corrective orthotics or toe spacers, in addition to appropriate shoes. These can help slightly realign the big toe and relieve the painful area.
Choosing the right footwear is a simple yet essential step in managing and potentially preventing hallux valgus.
The Role of Orthotic Insoles and Night Splints
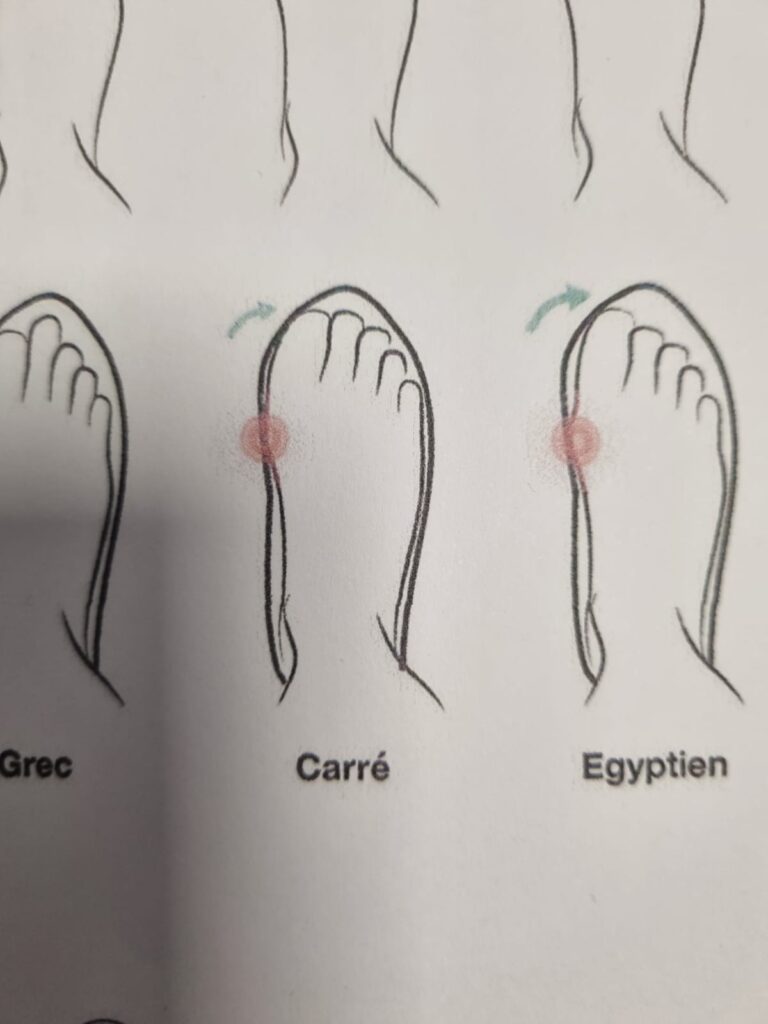
In addition to exercises and appropriate footwear, wearing orthotic insoles and night splints can play a preventive role in slowing the progression of hallux valgus.
These devices aim to restore better foot biomechanics and relieve tension on the big toe.

Orthotic Insoles and Night Splints
Orthotic insoles, prescribed by a podiatrist after a postural assessment, help correct plantar support.
They promote more balanced foot alignment and reduce excessive pressure on the forefoot. Depending on the foot type (high arch, flat foot, valgus), the insole is custom-made.
It may include arch support, reinforcement under the first metatarsal, or a cushion to relieve joint pain.
Night splints, on the other hand, are soft or rigid braces worn during sleep. Their goal is to maintain the big toe in a more natural alignment without applying force. While these devices do not correct an established deformity, they help prevent its worsening by limiting prolonged tension during the night.
Some versions can also be worn at home during rest periods.
When used together, insoles and splints help address postural imbalances and mechanical stress that contribute to the progression of hallux valgus. They also offer significant relief for those experiencing recurring pain.
The guidance of a healthcare professional is essential to adapt these devices to each individual case. When used correctly, they are a key tool in the prevention of hallux valgus, especially in cases of family predisposition or early signs of deformity.

Monitoring Progression: When to Consult a Specialist
Regularly checking the condition of your feet is a key part of preventing hallux valgus. The earlier the condition is addressed, the easier it is to slow its progression without needing surgery.
Certain early signs should raise concern: the appearance of a bump on the side of the foot or a gradual deviation of the big toe, recurring redness or inflammation, discomfort in shoes, or pain when walking. Even if pain is not present at first, a podiatric evaluation may reveal imbalances that require correction.
A consultation with a podiatrist or foot specialist is recommended as soon as these symptoms appear. The clinical exam is often supplemented with a weight-bearing X-ray to accurately assess the angle of toe deviation and the degree of joint deformation.
For at-risk individuals (family history, jobs requiring prolonged standing, athletes), an annual check-up is recommended. This helps adjust preventive measures and allows for timely intervention if the condition progresses rapidly.
A consultation becomes essential if the pain becomes intense or interferes with sports activities, or if it becomes disabling or affects the aesthetic appearance of the foot. It is also necessary when conservative treatments (insoles, exercises, proper footwear) no longer provide relief. In such cases, surgical treatment may be considered.
In short, it is better to consult sooner rather than later. A proactive approach helps prevent worsening of the deformity and preserves quality of life.
Conclusion: Act Early to Slow Hallux Valgus and Prevent Worsening
Hallux valgus is a common, progressive, and often underestimated condition. Yet simple measures can slow its progression and even avoid surgical intervention. Prevention is based on three essential pillars: understanding the risk factors, adopting a foot-friendly lifestyle, and consulting at the first signs.
Changing your footwear habits and incorporating hallux valgus prevention exercises are helpful steps. It’s also important to manage your weight, strengthen foot muscles, and use appropriate devices (insoles, splints). These actions allow for effective daily management. While these strategies won’t reverse the deformity, they often succeed in halting or slowing its progression and easing pain.
Patient involvement is essential: the earlier the intervention, the more lasting the results. In a society where prolonged standing and ill-fitting shoes are common, it is crucial to pay attention to foot health from a young age.
Finally, don’t hesitate to consult a specialist (podiatrist, sports doctor, orthopedic surgeon). This ensures personalized care and timely, well-informed decisions.
Preventing hallux valgus means investing in your comfort, mobility, and long-term quality of life.
FAQ – Hallux Valgus Prevention
Can hallux valgus go away without surgery?
No. Once the deformity is established, it does not spontaneously reverse. However, conservative measures like exercises, orthotic devices, and proper footwear can often slow its progression and relieve symptoms.
Is walking barefoot beneficial?
Yes, when done in a safe environment (clean, stable, natural surface), walking barefoot can be beneficial. It helps strengthen the foot’s intrinsic muscles, improve balance, and promote more natural posture. It’s a helpful addition to hallux valgus prevention—provided there’s no significant pain already present.
Are all heels bad?
Not necessarily. Moderate heels (4 to 5 cm) with proper support can even help stabilize certain foot types. It’s mainly high, narrow heels that are problematic—they increase pressure on the forefoot and contribute to big toe deviation.
Can hallux valgus be prevented in children?
Yes and no. While hallux valgus is rare in children, some signs (flat feet, instability, tight shoes) can promote poor development. It’s important to choose flexible, stable shoes with good support. If abnormalities are detected, a podiatrist should be consulted. However, hereditary or congenital deformities tend to progress inevitably.
How often should hallux valgus prevention exercises be done?
Ideally, they should be performed daily for 5 to 10 minutes. Consistency is more important than duration. During periods of pain or fatigue, they can be spaced out, but the best preventive effect comes with regular practice.