Informations on Foot & Ankle Surgery
Maison de santé pluridisciplinaire
5 promenade des Champs Plaisants, 89100 SENS
03 58 38 50 48
Polyclinique
Sainte Marguerite
5 Av De La Fontaine Ste Marguerite, 89000 AUXERRE
03 86 94 51 71
- C.E.S: Certificate of Special Studies in Sport Medicine and Biology and
- Higher Education: Certificate of Higher Education in Biomechanics of the Musculoskeletal System and Kinesiology.

Most common diseases
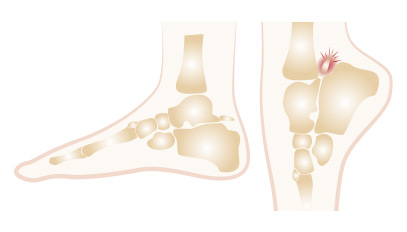
Hallux valgus, commonly known as a bunion, is a painful deformity. It can make wearing regular shoes difficult and, in the early stages, the pain may become unbearable.
This condition affects the fifth toe, the smallest one. Symptoms begin with pain and stiffness. Over time, a hyperkeratosis (thickened skin) develops on the dorsal part of the toe.

This condition affects one or more toes. In the initial stage, the deformity is reducible, but over time, it progresses to stiffness.
This deformity involves the distal metatarsal epiphysis. The physiological architecture of the metatarsal heads forms a concave curve.

This condition is more common in men. It manifests as pain and/or stiffness in the big toe. It can sometimes cause limping and difficulty wearing shoes. The shoe becomes uncomfortable to wear and causes friction against the bone.
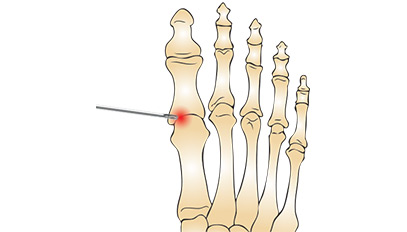
It's the formation of a neurologically derived swelling, 4 to 8 mm in diameter, originating from an interdigital plantar nerve located in the metatarsal space. Mechanically induced, neuroma is exacerbated by tight footwear and is more common in women. It may regress spontaneously.

It is the largest and longest tendon in the body. Essential for walking, it has a propulsive effect and therefore must be very powerful. Also called the calcaneal tendon, it extends from the calf muscle and inserts into the calcaneus. It spans two joints: the knee and the ankle. It connects the triceps muscle to the heel.
It is a surgical procedure performed through percutaneous methods (2 to 3 puncture incisions), using an optic and camera to visualize the various compartments, thereby allowing a systematic exploration for diagnostic confirmation and therapeutic interventions.
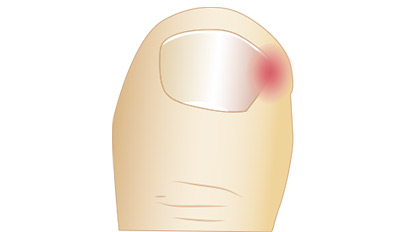
It's a wound caused by a fragment of the nail penetrating the surrounding skin, which can vary in inflammation and infection levels, manifesting as redness, pain, and varying degrees of serous or purulent discharge. This condition commonly affects the big toe nail and can occur on the side or front of the nail.
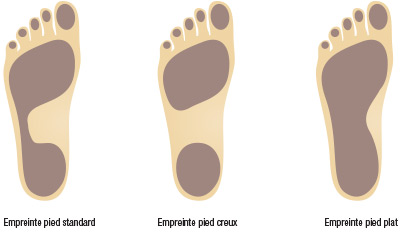
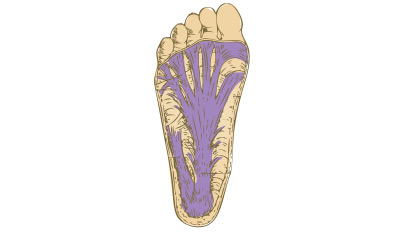
It's a foot with a widened footprint. Clinically, the inner arch is less pronounced, or even absent. Radiographic assessment shows normal axes, and in some advanced cases, there may be a misalignment of the bones of the first ray with the talus, the first cuneiform, and the navicular bone, with a downward collapse of the line on the profile.
Mini-invasive and percutaneous surgery in forefoot
Mini-invasive foot surgery is a surgical technique that, as the name implies, relies on small incisions (not exceeding 1 to 2 cm) to perform surgical procedures typically conducted via broader approaches.
This approach entails two consequences: a) the surgeon may not have full visual access to the surgical site, and b) specialized surgical instruments of appropriate size and design are necessary.
Consequently, this type of surgery is only performed using these tailored instruments and specific lighting systems dedicated to this purpose. This includes a form of televisual radiography, enabling real-time visualization and monitoring of each movement’s effects. The aim is to ensure precise control in areas not directly visible to the surgeon.
Limited approaches (10%)
Few tissue detachments,
Faster healing, quicker recovery,
Lower complication rates:
Including fewer infections, less neuro-algodystrophy (or Complex Regional Pain Syndrome = CRPS),
Less precision, requiring television radiography
Increased risk of radiation for healthcare providers,
Paradigm Shift:
Mini-invasive and percutaneous surgery in foot surgery is to visceral surgery what Laparoscopy is to Visceral Surgery,
Mini-invasive and percutaneous surgery is to Meniscectomy what Arthroscopy is.
In young individuals
In the elderly:
In major deformities
In minor deformities
Orthopedic surgeons skilled in MIS techniques.
In a dedicated setting with appropriate instruments and adequate training, along with a low radiation amplifier.

Learn more ...

Hallux Valgus and Index Minus
This article is intended for both patients and healthcare professionals. It focuses on the relationship between hallux valgus and index minus—two often-associated yet not always
The pathologies described and the treatments indicated in various paragraphs of this site are merely indicative. Only a professional can advise you and a surgeon specialist explain to you during a consultation your pathology and choose, if necessary, with you, the appropriate treatment and the most adapted to your own organization and your own particular case.
It is now accepted that smoking increases the risk* (skin and bone) in the case of foot surgery by a factor of 2 to 10. Smoking thus leads to a disruption of the natural vascular phenomenon* of wound healing ( = Scarring), which can lead to a disunion of the scar, or even a cutaneous necrosis* to which is added a risk of delay or even lack of consolidation of the bone. Therefore, it is strongly recommended to stop smoking 6 weeks* before surgery and 6 weeks after.
* These risks are: a higher rate of post-operative complications, including disorders of wound healing (incisions). Cicatrization is the natural phenomenon, which allows surgical incisions to heal by closing and which tobacco obstructs or even disturbs. If there is a risk of post-operative edema (varicose veins, varicosities, venous disturbances, and in particular any disorder in the return of blood to the veins), then the risk associated with smoking is increased by blood stagnation In the operated areas and by the appearance of prolonged edema, which by pulling on the sutures of the incisions, slows down the normal process of scarring.