Hallux valgus, commonly known as a bunion, is a frequent forefoot deformity, affecting mainly women.
It is characterized by the deviation of the big toe toward the outside, leading to a painful bony bump on the inner edge of the foot. Over time, this condition can interfere with walking, make footwear difficult, and significantly impact quality of life.
In the early stages, conservative treatments such as custom or over-the-counter orthotics and adapted shoes can provide temporary relief. However, when these solutions are no longer effective, surgery remains the only option for lasting and effective correction.
In summary, bunion surgery is intended for a wide range of patients, with treatment tailored to each individual’s clinical situation, needs, and expectations.
Percutaneous surgery is also suitable in cases of recurrence, even after multiple operations. It is particularly indicated when skin adhesions or tendon retractions are present. Moreover, this technique minimizes incisions and allows a personalized “à la carte” approach depending on the deformity of each toe.

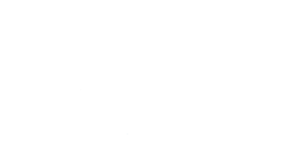
Example:



Procedure performed:
- Percutaneous surgery on the 2nd, 3rd, and 4th toes
- Percutaneous osteotomy of the first phalanx of the big toe
- Mini-invasive (1 cm) lengthening of the long extensor tendon of the big toe
- Tenotomy/lengthening of the extensors using the Green technique
Improved healing and aesthetic outcome
Today, percutaneous hallux valgus surgery is highly valued by patients and is considered a modern alternative to traditional open techniques. Less invasive, it is performed through very small incisions, which reduces post-operative pain, scar size, and recovery time. It provides both functional and aesthetic benefits.
This technique, developed in the USA around 1985, was introduced in Spain in 1994, and later adopted in France in the 2000s.
It is performed by orthopedic surgeons specialized in foot surgery, who, thanks to expertise in minimally invasive techniques, can offer individualized care to help patients regain comfort and mobility.
Minimally Invasive Surgical Techniques for Hallux Valgus
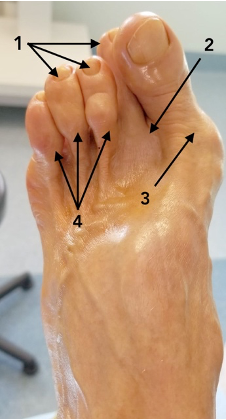
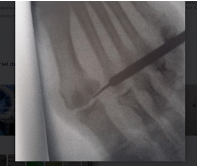
Percutaneous hallux valgus surgery corrects the bony deformity through very small skin incisions (2–5 mm), using specific instruments under radiological guidance. The aim is to limit soft tissue damage, reduce post-operative inflammation, and promote faster recovery. Several techniques exist depending on the severity of the deformity and the surgeon’s preferences.
- MICA (Minimally Invasive Chevron and Akin): Combines two osteotomies, one of the first metatarsal (Chevron) and another of the proximal phalanx (Akin), offering precise three-dimensional correction.
- Bösch / SERI (Simple, Effective, Rapid, Inexpensive): Involves a simple osteotomy of the first metatarsal, stabilized with a temporary pin. Recommended for moderate cases, known for its simplicity and speed.
- Other techniques: PERC (Percutaneous Extra-articular Reverse Chevron), PECA (Percutaneous Chevron Akin), and MIS (Mini-Invasive Surgery). These allow direct bone correction through the skin, usually without the need for permanent internal fixation.
Despite their differences, all these techniques share the same goal: to realign the big toe with less invasive surgery, better tolerated by patients.
Minimally Invasive Approaches to Hallux Valgus Recurrence: Indications, Procedure, and Outcomes
Compared to traditional open surgery, minimally invasive surgery offers several major clinical advantages:
Reduced pain: Small incisions and better preservation of soft tissues (muscles, tendons, nerves, vessels) significantly reduce inflammation and post-operative pain, often avoiding the need for strong painkillers.
Better healing: Smaller wounds lower the risk of infection, skin complications, or unsightly scars. Aesthetically, results are superior, especially valued by younger or active patients.
Faster recovery: Walking is usually possible the day after surgery with a post-operative shoe. Patients regain autonomy earlier, return to work sooner, and resume light sports by the 6th–8th week. Running and forefoot-intensive sports (football, tennis, basketball, volleyball) are allowed from the 12th week.

Preserved mobility: These techniques reduce stiffness and long-term mechanical complications. Often, both feet can be operated on within a few weeks, under better comfort conditions.

In short, this modern approach greatly improves both the surgical experience and functional results, while minimizing patient constraints.
Benefits of Minimally Invasive Approaches to Hallux Valgus Recurrence
Minimally invasive bunion surgery aims to:
- Realign the big toe
- Remove the bony prominence
- Reduce pain
- Improve foot aesthetics and functionality
Results are generally very satisfactory, provided that surgical indications are well established and post-operative care strictly followed.
Patients usually notice:
- Significant pain relief within days
- Gradual reduction of walking discomfort as healing progresses
- Progressive realignment of the toe, restoring better weight distribution on the forefoot
Aesthetically, the disappearance of the bunion improves foot appearance, making shoes more comfortable and reducing friction.
In the medium to long term, most patients recover near-normal foot function and resume all activities, including sports and prolonged standing. The recurrence rate remains low, provided the surgery is well performed and risk factors (inappropriate shoes, excess weight, postural problems) are addressed.
Complications are rare but may include stiffness, overcorrection, recurrence, or infection. These are usually preventable with regular follow-up and good communication with the surgeon.
Preparation and Post-Operative Follow-Up
The success of percutaneous hallux valgus surgery depends on both surgical technique and careful preparation/follow-up.
Before surgery:
- Preoperative consultation with clinical exam, X-rays, and lab tests
- Adjustment of medications if necessary (e.g. anticoagulants, anti-inflammatories)
- Planning of rest and daily life adaptations for recovery
On surgery day:
- Usually performed under local-regional anesthesia
- Patients typically go home the same day
After surgery:
- Post-operative shoe worn for several weeks
- Regular follow-up visits to monitor healing and alignment
- Dressing care, gentle physiotherapy, mobility exercises
- Strict adherence to post-op instructions (special footwear, limited exertion, hygiene)
Gradual walking resumes early, and sports typically restart around the 6th week depending on progress.
Preparation and Post-Operative Follow-Up: Key Steps to Optimize Results
The success of minimally invasive approaches to hallux valgus recurrence depends not only on the surgical technique but also on careful preparation and attentive post-operative follow-up. These steps are essential to ensure a rapid recovery and reduce the risk of complications.
Before the operation, a preoperative consultation with the surgeon is crucial. It allows for a full assessment: analysis of the deformity, imaging tests (X-rays), blood tests, and an evaluation of the patient’s general health. In many cases, medical treatments such as anticoagulants or anti-inflammatory drugs must be adjusted. It is also recommended to plan for a period of rest after surgery and adapt daily activities accordingly.
On the day of the procedure, local-regional anesthesia is usually performed. This ensures quick recovery and allows the patient to return home the same day. After surgery, wearing a special post-operative shoe is required for several weeks. This protects the bone correction while enabling immediate, pain-free weight-bearing.
Post-operative follow-up involves regular consultations with the surgeon to monitor healing, check alignment, and adapt the resumption of activities. Dressing care, light physiotherapy, and mobility exercises are recommended to prevent joint stiffness.
Strict adherence to post-operative recommendations is key to the success of bunion surgery. This includes wearing the prescribed shoe, limiting physical strain, and maintaining good local hygiene. Gradual walking can be resumed as healing progresses, and sports activities are usually allowed from the 6th week onward, depending on recovery.
In summary, good preparation and close follow-up maximize the benefits of minimally invasive surgery for hallux valgus recurrence. They help achieve high patient satisfaction and long-lasting recovery.
Percutaneous Hallux Valgus Surgery: A Modern and Effective Solution
Percutaneous surgery for hallux valgus recurrence represents a major advance in the treatment of this common and disabling condition. Based on innovative, precise, and minimally invasive surgical techniques, it corrects bunions while reducing pain, scarring, and recovery time.
Among the most widely used methods are the MICA, SERI, and other percutaneous techniques. These are tailored to the degree of deformity and the patient’s profile. The goal remains the same: to provide a customized correction that respects foot morphology and lifestyle.
This approach, combined with careful preparation and rigorous follow-up, allows for a rapid return to walking. It greatly improves daily comfort and provides valuable aesthetic results.
If you suffer from hallux valgus that interferes with your daily life, consult a foot and ankle orthopedic surgeon specialized in minimally invasive approaches to hallux valgus recurrence. With personalized care, you can regain mobility, restore comfort, and significantly improve your quality of life.