Hallux Valgus
Complaining of foot pains is very common. A “new bone” appears sometimes, at the basis of the great toe. Wearing the same shoes becomes difficult, and high heels shoes becomes unaffordable. We call this disease “Bunion”. Bunion disease occurs with a small deformity getting bigger or by a pain or both. In some cases, it starts by feeling that the shoes are not comfortable anymore.


Hallux valgus in 26 questions:

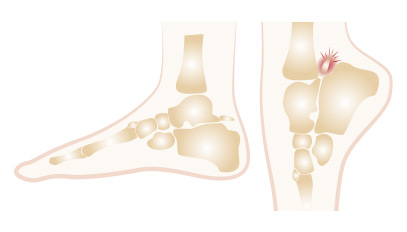
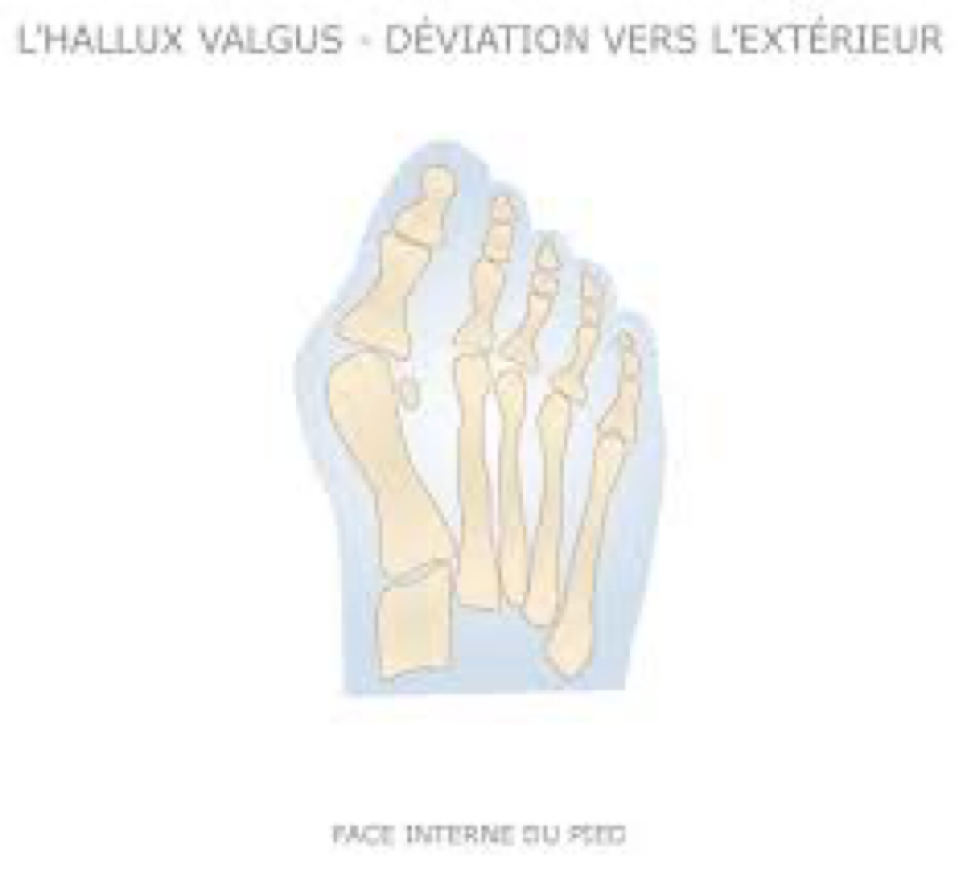
It is a sometimes painful distortion of the foot called « hallux valgus », which means that the big toe is exaggeratedly outwards, oriented to the outside of the foot. With an enlarged forefoot. Why and where does this distortion come from? Because the first ray: which is made of the first metatarsal and 2 Phalanges: the 1st metatarsal. Diverges from the second metatarsal and the large toe, which consists of two phalanges, moves outwards, and that there is a partial relaxation of the tendons, capsules, and aponeuroses. The « bunion » is not a new bone that has grown. This « bump » under the skin rubs against the shoe and creates a conflict at the origin of the pain, there is associated a redness called« bursitis ». Bursitis is therefore the term which designates the formation between the skin and the bone of a small pocket which can ignite, sometimes contain some liquid.

This divergence between the 1st and 2nd bone radius affects 10% of the population, especially women (the majority of cases). The cause of this deformation is multiple and complex, it is acquired in 60 to 70% of the cases and innate in 30%. The shoe can be incriminated in the acquired forms but it is not only because of the shoe. It is also the shape and mobility of bone tissue and soft tissue that play a part and contribute to the creation of this deformity which becomes painful. The components that create or precipitate the creation of the deformity are: flat foot, big toe (Egyptian foot), hallomegaly, family history (30%) or overweight. This can also occur on hollow feet. The shoe precipitates and / or aggravates the relaxation of the tendons and the capsule.

Operation of the hallux valgus does not necessarily prevent distortion of the other toes. A toe is independent and can endure relaxation and musculo-tendinous contractions. Mechanically the big toe can clash with the 2nd and push it out, precipitating or aggravating the formation of a second toe grip. Once the hallux valgus is operated, the other toes can stabilize or continue the progression of the deformation, necessitating sometimes another specific intervention dedicated to this situation. However, it should be noted that some surgical techniques re-balance the distortion of the forefoot better than others, which can stop or decrease preventively the deformation of the other toes called « laterals ».

There is no definite rules. No precise age for surgery, we just have to wait, in the young, if possible, the end of growth. The extreme ages range from 15-16 to 86 -87 years, mostly around 50 -55 years of maximum discomfort. The indication of an operation does not depend on age. It depends on the embarrassment to the shoe and the pain that exists with the deformation of the big toe.

Indirectly answered in question 18. The partial support period of the forefoot lasts from 3 to 4 weeks, complete support is then allowed and bone consolidation usually occurs between the 6th and 8th week.
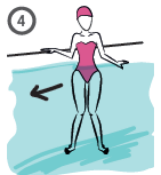
Unnecessary immediately after surgery, becomes useful after ablation of points and especially between the 3rd-4th week and the 6th-8th week. For self-re-education which involves mobilizing oneself in flexion / extension several times a day the toes is highly recommended as well as an ascending massage between the thumb and the index of the root of the toes to the calf, but when stiffness occurs, the solution is rehabilitation and auto-rehabilitation by exercices like wolking in aquatic environment ( swimming pool).
quatic sessions can be performed by the patient alone in a pool where they can stand, according to the following program.
This should be repeated 2 to 3 times per session (1 hour and 15 minutes to 1 hour and 30 minutes), and done 3 times a week for 3 weeks: that is, 9 to 10 sessions.




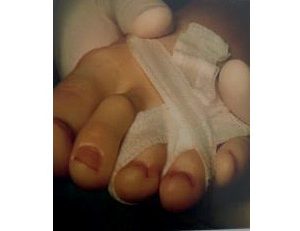
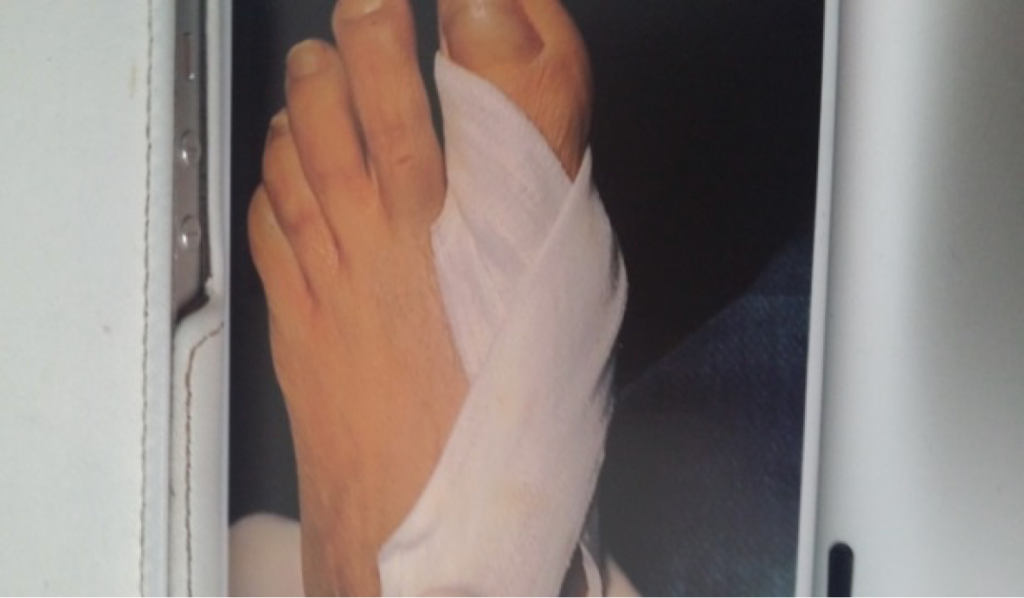
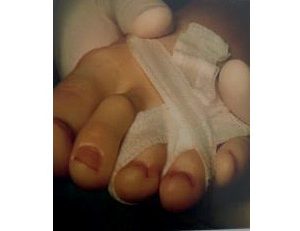
a) The first dressing is done by the surgeon between the 1st and 3rd week, then once every 2 to 3 days until healing.
Dressing: Compresses are 10 x 10 cm, of which 3 are woven, unrolled, and moistened. The rest of the compresses are dry, woven, and unrolled.
The dressing should not be changed before the 21st DAY. There is no pus…, there is no maceration….
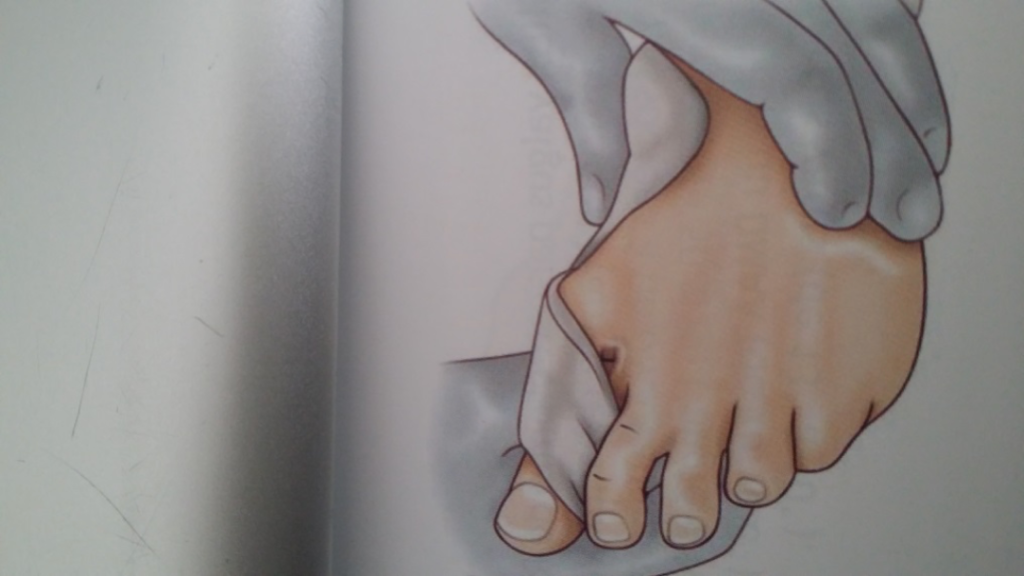
Principle:
10 woven 10×10 cm compresses, of which (3) are moistened, folded lengthwise, wrung out and tied around the big toe.
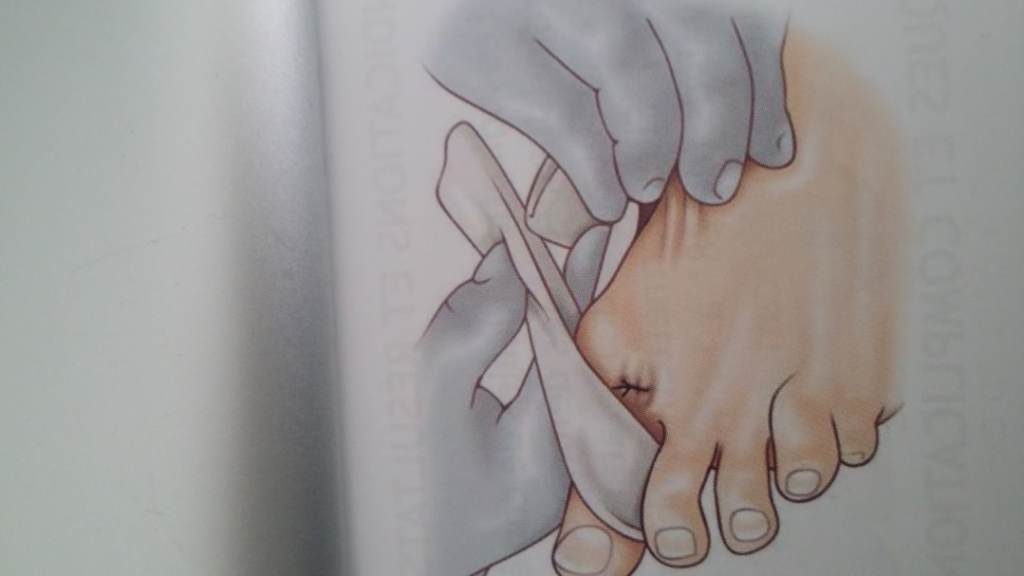
(4) Unrolled and placed in a circular manner.
(1) 10 cm Velpeau bandage.


b) A preventive treatment for thromboembolic complications is prescribed; it is not mandatory in foot surgery, especially if the patient walks the day after surgery and applies weight. However, it is customary to cover this risk with a daily subcutaneous injection of LMWH (Low Molecular Weight Heparin) for 10 to 20 days, maximum 30 days, especially if the patient has risk factors for thrombosis. Other treatments are available in tablet form: Pradaxa™ or Xarelto™.
c) Follow-up visit. This takes place between 1 and 3 weeks to check the wounds and weight-bearing. In any case, there is a follow-up at 6 weeks with a control X-ray to assess the evolution of bone healing from osteoclasis and/or osteotomies.
d) Wearing normal shoes? This can be done from the 4th week onwards, and if the foot remains swollen, from the 6th week. Edema is the enemy of the shoe. It limits the return to normal heating. It is specific and depends on each person, the condition of their venous return, and generally the condition of their veins. The first shoes should be wide with a rounded toe, with Velcro or laces, and one or half a size larger than the initial size. It should be noted that the old shoe reproduces the deformation and should not be worn, in principle. High-heeled shoes after bunion surgery are allowed even though this type of shoe is not very physiological.
e) Sick leave: Sick leave depends on the severity of the procedure, which depends on the extent of the deformity. Other criteria also influence the duration of sick leave: the patient’s weight, age, and type of activity, as wearing safety shoes is a crucial element in this decision. Sick leave ranges from a minimum of 1 month to 2.5 months. Simultaneous operation on both feet requires a similar duration, not longer.
f) When can you drive again? Driving is allowed as soon as the post-operative shoe is discarded and there is good mobility of the toes, typically 4 to 6 weeks.
Bandaging after Hallux Valgus
g) Resuming sports? After the 6th week of recovery, it becomes possible to gradually resume sports, focusing on activities that do not stress the foot much: flat cycling or swimming once the wound has healed. It is advisable to wait 3 to 4 months before returning to sports that involve pressure on the forefoot and require active walking.
h) Same sports as before? The surgical operation does not alter the capacity of the muscles and the bone affected during the procedure. After complete consolidation (after 10 to 12 weeks), the patient can resume previous sports activities, even competitive ones.
i) Question of recurrence? The question is legitimate, and the risk of recurrence is real. It depends on the quality of the correction, post-operative footwear, and the severity of the deformity. Some believe that if the correction is done at an advanced stage, there is little chance of the deformity returning, whereas if it is done at an early stage or a young age, there is still potential for recurrence. It is difficult to settle this debate, but it exists, and it is important to know that recurrence is possible and that post-operative footwear plays a role in this.
j) Removal of hardware? Beyond 3 months, bone consolidation is generally achieved, and the orthopedic hardware is no longer necessary. If it causes discomfort due to rubbing in the shoe, it can be removed, but a waiting period of one year is recommended. Some use absorbable pins that do not need to be removed as they dissolve within 9 to 18 months.
k) Does removal of hardware increase the risk of recurrence? No, osteotomies must be fully consolidated. After the 3-month period, bone consolidation is achieved, and the orthopedic hardware is no longer necessary. If it is removed, the bone retains its position, and removal does not increase the risk of recurrence.





There is no urgency to operate a hallux valgus and all those who do not are operated, obligatorily (except inflammatory bursitis, ulcerative, with serous or purulent discharge). An intervention can be justified only if the patient is embarrassed, functionally with a pain that becomes continuous and / or disabling, with a dilemma to put on. Surgery should never be performed for aesthetic reasons or for purely foot width reasons or aesthetic finesse or preventive. The intervention is always possible whatever the deformation.

One can delay the evolution and prevent the consequences of the imbalance with cloth or soft leather shoes, with rounded toe giving enough space for the toes avoiding the seams facing the zones of friction. The shape of the sole especially if the foot is flat can also be important. Wearing a small sole with inner arch support can make the footwear comfortable. By changing the load distribution on the other toes. It will be performed by a professional graduate in podiatry

There are protections called « toe separator » or « spreader » or silicone « spacer » that can temporarily alleviate. Just as there are « orthoplasty » or nocturnal reduction orthoses, which are protective silicone gel products, and which also can temporarily alleviate the pain, but this does not really change the evolution of the deformation of the fat toe. They can relieve, delay a little and in some cases prevent degradation and aggravation.

There is no known and validated medical treatment that corrects the deformity. Only surgery can treat the pain by reducing the deformity and repositioning the tendinous attachments. However, having hallux valgus does not necessarily mean surgery is required. The decision also depends on the degree of discomfort, tolerance, and especially the severity of the pain. The shoe deformation, the condition of the sesamoid bones, and their positions also factor into the decision. Surgery is not performed on a lesion, an X-ray, or even a deformity, but on a patient with their medical history and pathologies. The evaluation of this history and the risk-benefit balance assessed with the surgeon and the anesthesiologist form the basis of the surgical indication and the nature of the operative procedure. Deciding to operate on hallux valgus should never be taken lightly, as complications can arise, such as hypercorrection leading to postoperative hallux varus (as shown in the photo above).

The criteria are numerous, the taking into account of the antecedents is essential, but the specific decision rests on essentially 3 criteria: The functional discomfort to the heating which is paramount in the decision (motivates half of the decision). Pain on the level of the onion or on the lateral toes which is a key element of the surgical indication. Is it disabling? Does it impotence? The importance of the deformation which is an element but secondary (15%). According to the American Orthopedic Foot and Ankle Society (AOFAS) criteria, plastic or aesthetic motivation should not be included in the components of a surgical decision.
There are three types of anesthesia: general anesthesia, rachiesthesia (or epidural equivalent), and loco-regional anesthesia, also known as nervous or neurological peripheral anesthesia, or so-called truncular anesthesia. It is an anesthesia often advised because the patient is asleep only from the knee to the foot. This anesthesia does not disrupt the body and has a post-surgical analgesia lasting several hours. If bilateral surgery is performed, general anesthesia or spinal anesthesia will be more readily available.
It is recommended to operate one foot after the other. The pain is less and it is easier to move when one foot is limited and the other is normal or functional (postoperative shoes being unbalanced).
It also depends on the size of the deformations and the type Intervention. In the case of bilateral simple hallux valgus, Possible to operate both feet at the same time. But the experience patients attests that this is more challenging. If the deformation is Complex with many operative gestures on several toes and metatarsal rays, it is recommended to operate one foot then the other with 2 weeks to 3 months of delay, depending on the case.

The duration varies according to the operating method, the importance of the deformation and the number of toes to be operated. For a simple hallux valgus, the duration of the gesture is 30 to 45 minutes. On a complex foot, it is twice as long, but the absence of the patient from his room lasts 2 to 4 hours because there is preparation and passage in the recovery room.

The bad reputation (the surgery of the foot is said to be very painful and trying) emanates from the heavy and wide techniques with an analgesia post-operative ine cace, or even absent. At present, anesthesia has a range of analgesic protocols, but most often, by offering locoregional anesthesia, there is an e and analgesic which lasts several hours after surgery and which can, if requested by the surgeon, and patient accepts it, leave a catheter to inject analgesics and anesthetics in situ for 24 to 48 hours.
And since the really painful phase lasts only 48 hours, the problem is solved, but each one does not react similarly to this analgesia and this type of anesthesia. Then analgesia is supplemented by powerful analgesics such as morphine drugs or their equivalents.
The answer is NO. There is not one univocal technique for all hallux valgus, because there are several types of interventions:
- Bone gesture only,
- gesture on the soft parts only,
- a mix, of the 2,
- In the open surgery, or
- With closed hearth,
- With a wide osteotomy, over the entire length of the metatarsal,
- oblique or in Z called SCARF
- or limited : in « bevel » or in « chevron », with acute angle or not,
- Seated at the proximal metaphysis (Lapidus) or distal, respecting the articulation or not (Keller-Lelièvre), associated or not with a gesture on the phalanx (Atkin).
The type of intervention must depend on:
- The value of the angle M1-M2 (which is normally from 6 to 8 °, maximum 10 °), and The value of the angle M1-P1 (which is normally from 10 to 12 °, maximum 15),
- The morphotype of the foot,
- The patient’s general condition like age, bone status, presence of diabetes or not, insulin-dependent or not, distal vascular state
- the practice of the operator.
And each of the criteria can present alone or together, affecting the choice.
Most of these techniques are to re-center the bone and to reduce the value of the angle M1-M2. And the value of angle M1-P1 must also be reduced.
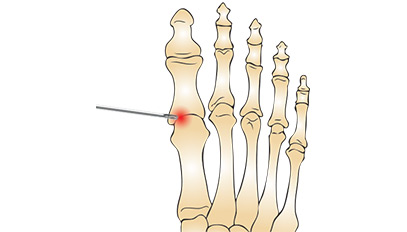
It is possible to proceed by what we call an osteoclasy (bone fragilisation) or directly with an osteotomy (section of the bone, with a saw). That is to say, in order to correct the axis, one proceeds in various ways. In fact, it is necessary to weaken the bone by several perforations, to leave a bone bridge, and it is by manually supplementing the osteoclasis that the axis of the bone is raised. This can be done by a mini-approach (known as « buttonhole » or « punctiform » or « fly » giving scars 2 to 8 mm long, (this is the so-called « percutaneous » technique) Or by incising to minima (ie mini-approach), also called mini-invasive. This action lasts from 30 to 70 minutes depending on the case and will allow by small cutaneous openings to introduce surgical instruments and to use tools that will allow thanks to the control obtained by the amplifier of brilliance (which is a kind of » Screen television equipped with a radiological source that shows the bone as a cliché, it is also called Fluoroscopy), to carry out the intervention without large incision of the skin
By this means, contraction of the tendons can be severed and the bones of the foot can be affected: the metatarsal and the phalanges, (of the big toe and of the other toes if they are deformed too).
Si la déformation est conséquente et s’associe à une atteinte latérale des autres orteils, on réalisera peut être u
If an « arthrodesis » (blockage) of the MTP (metatarsophalangeal) joint of the big toe is required because there is subluxation or advanced osteoarthritis, the incision may be wider. Some surgeons are able to do this « blocking » percutaneously as well. Finally, this blocking may be necessary because of age, osteoporosis or recurrence of deformation (iterative surgery, also called surgery of recovery) or by stiffness.

These surgical approaches are based on the same principles, they will be adapted to the morphotype of the foot, the presence of a flat or hollow foot, the orientation of the back foot, age, the presence of a front – anterior round foot (APRA: deformation of the forefoot in convex form instead of being concave). To the importance of the deformation, to the association of several deformations of the other toes adjacent, also called lateral.
Not really because the answer is YES and NO. Because surgery is always possible no matter how important the deformation. The time of consolidation (that is, the time of healing of the gesture made on the bone) is roughly the same regardless of the nature of the act. And the convalescence period is almost always the same: 4 to 6 weeks. But more limited deformation and more the surgical procedure is simple. The surgeon adapts his technique to deformation. But it should not be Operating a hallux valgus early, the operation will prevent the other toes from deforming. Moreover, a recurrence of the distortion of the big toe remains possible further.

No. The quality of the bone does not really intervene in the result and the osteoporosis does not prevent bone consolidation

No, foot deformities cannot be corrected by any method other than surgery, such as laser. There might be a misunderstanding because in recent years, minimally invasive techniques known as "percutaneous" surgery have been introduced in France, where operations are performed through small incisions. These methods have been used for over 25 years in the United States and more recently in France. For this type of surgery, no "laser" is used but rather specific smaller instruments, small burrs similar to those used in dentistry, and special working methods under a fluoroscope (an imaging device that visualizes the bone like an X-ray source).

The duration of hospitalization varies according to the technique, the deformations corrected and according to the practices of the operator. The procedure can be performed in ambulatory surgery (without hospitalization) if the gesture is simple or minimally invasive and / or percutaneous. The hospitalization may last 24 hours sometimes 48 for certain techniques, maximum 3 for complex feet covering all the radii of the foot or recurrences.

The rising takes place the following day with mobilization in the chair. With some rare exception, it is also the day after the intervention that you can take the first steps, with a shoe that allows partial support of the forefoot.

At the beginning, with the help of a shoe that completely discharges the forefoot (BaroukTM shoe type) or better that which allows partial support (with a so-called buffer Blotting, SOBER® brand or PODALUX®) which allows to preserve a good autonomy. The use of a cane can be advised to maintain balance if there is total discharge of the forefoot.
To conclude : Hallux Valgus
In conclusion, hallux valgus is a common benign condition that can become very painful and disabling, and it can be treated through open surgical procedures (with incisions of 6 to 12 cm, especially for the SCARF technique), minimally invasive surgery, percutaneous surgery, or a mix of both.
Percutaneous or minimally invasive surgery does not use lasers but rather specific instruments and is performed under fluoroscopy (an imaging amplifier). The results of both techniques are comparable, with a slight advantage to percutaneous surgery because the smaller incisions heal faster, hospitalization can be shorter, and recovery can be slightly quicker. However, the surgeon’s experience and familiarity with a particular technique remain important factors in the decision and choice of method.