– frequent recurring illnesses
Corns, calluses, and hyperkeratosis are common skin conditions affecting the foot. These lesions usually develop as a response to repeated friction, pressure, or abnormal mechanical stresses on certain areas. Corn callus and hyperkeratosis can cause pain, discomfort, and difficulty wearing certain shoes.
The skin is a “tissue” like another, it envelops the body, it is of different thickness depending on the localization, very thin at the level of the eyelids (a few mm), thicker on the trunk and hips, it reaches 8 To 10 mm at the level of the sole of the foot. Mobile on the back of the hand and at the level of the eyelids, it is fixed and “adherent” at the level of the plant.
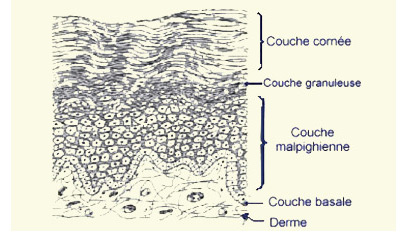
In continuous renewal, the skin’s so-called epidermis is made up of layers of cells, each layer is made up of cells spread out, next to each other and affixed like tiles whose major axis is parallel to the area; These cells become flattened, and as the layers rise towards the surface, they lose their thickness and eventually dry up and fall. The surface layer is called the stratum corneum. And the skin that falls is sometimes called the “horn”. (Fig. 1)
The “biomechanics” of the skin
The skin is a tissue like any other, its first quality is elasticity, it can withstand elongations when losing weight and return to the initial shape if the individual loses weight. In some cases of deformity, this elasticity is exceeded, and the skin can “crack” giving “stretch marks”. On the moving regions, facing the joints of the fingers or toes, the elasticity is even greater. The adhesion to the deep tissues is another mechanical quality, light on the back of the hand, it is very adherent to the level of the sole of the foot. The specificity is that it is the envelope of the body, the whole body (except in regions where there are orifices or the skin is continuous by mucous membranes) and therefore it has several roles:
- Body protection
- Participates in “thermoregulation”
Mechanical Reason
When the skin is urged, by repeated pressures, it and always reacts in the same way. If the friction is seated on a moving area, such as facing a joint, redness forms in front of the joint. Due to the movements, a detachment takes place, a “pocket” is formed which eventually contains liquid, and then constitutes a “bursitis”. Sometimes, especially if there is no mobility in relation to the joint, the friction creates more layers of cells, and the skin responds to the mechanical stress by increasing the number of layers of cells. It ends up forming thick zones, called zones of hyperkeratosis.
Corn, callus, and hyperkeratosis:
Additional informations
Corn on the Foot
A topographical term, a “corn” refers to an area of skin irritation characterized by thickening, making it more resistant. Corns develop due to repetitive friction. They can occur following an inflammatory bursitis or form directly, essentially representing the “dry” form of bursitis. Pain accompanies either the inflammatory process or the formation of a keratosis.
Treatment typically involves local pedicure treatments, promoting comfortable healing, toe mobilization, and, if necessary, wearing orthoplasty or silicone fabric to reduce friction. Surgical intervention may be required if conservative measures fail, but simple excision carries a risk of recurrence. Etiological treatment through surgical correction of the deformity is the most effective way to reduce the risk of relapse.
The aim of surgical intervention is to eliminate friction, with percutaneous surgery being particularly well-suited to address this pathology.

Plantar Callus
Topographic appellation the “durillon” or Plantar Callus is an area of suffering that is to say, thickening of the skin to make it more resistant, it is a hyperkeratosis, a horn, and its topography gives it the name of the callus. It never or almost never follows a bursitis. Inflammatory. On the other hand, it can be complicated by a viral superinfection by a wart called “plantar wart or vulgar wart”. On a diabetic foot with ischemia and / or neuropathy, it can give rise to a “plantar perforating disease”
Treatment: medical and preservative par excellence, its cause is “in essence” mechanical: a baropodometric study will necessarily show a zone of hyper support. The mandill must disappear if the supports are well distributed, and this is done by the combination of an orthesis associated with a comfortable footwear. Baro- podometric examination with and without a soles if it is done two months after wearing soles made to measure, can reflect this distribution of supports. Failure in spite of well-made soles and which distributes well the supports, can push to pose a more radical treatment: surgical.
Percutaneous surgery is ideally suited to this condition. It will never be plantar, it will be etiologic, and it will correct a convex foot by a DMMO (or in French OMMD: metatarsal metatarsal disc osteotomy).

Treatment of hyperkeratosis
Painful or not, a hyperkeratosis (even small) must be the subject of a conservative medical treatment, which is first of all a symptomatic treatment, followed in case of failure or recurrence, a radical, etiological treatment, Usually surgical.
The Conservative Medical Treatment, essentially symptomatic, consists of:
- A comfortable footwear: Because the problem is not the deformation, it is due to the repeated rubbing, the shoe, which exerts and causes the reaction of the skin, hence the need to wear a comfortable shoe.
- Creams, ointments and solutions: skin thickening and desiccation (hyperkeratosis is always dry, very dry) causes hardening, creation of a keratoma and sometimes the perforation of the latter, generates phenomena painful. The application of moisturizing and / or exfoliating creams can solve the problem.
- Pedicure: is essential when the lesions persist, it consists of an excision of the “horns” in the hope of seeing them disappear thanks to an associated treatment like foot orthoses and / or a change of shoes.
- The orthosis or more precisely Orthoplasty: is very useful to distribute the pressures and decrease the zones of hyper support. It must help to limit or even reduce the calluses.
Treatment of the cause or etiology is most often surgical and is limited to solving the mechanical problem it is a treatment which in the majority of cases is percutaneous or minimally invasive.When the medical treatment has failed or when the lesion recurs and Becomes chronic, the cutaneous lesion associates with an “irreducible” deformation.
It consists, at best, in correcting the deformation or at times merely reducing the irreducible appearance by making the toe mobile and the possibility in the shoe of avoiding friction of the boot. It associates, on the card, one or more of the following acts:
01
Tenotomy
From the extensor of the extensor of the toe when the toe is retracted. Made intra-synovially, with a “beaver”, it is done percutaneously. It can relate to the flexor tendons Flexor (CF) and Long Flexor (LF), also makes to the “beaver” and does not require suture. Indicated in the toes of the toes or the “clinodactylies”.
02
Tendon elongation
A “Z” elongation with a fine nonabsorbable suture is indicated percutaneously or “open”, especially for large tendons. This is the case of the extender of the big toe.
03
Capsulotomy
This is the section of the joint capsule. In a graft, for example, the articular capsulotomy of the inter-phalangeal articulation is sometimes necessary, it is done by the plantar way.
04
Osteotomy
This is the section of the bone for axial correction, which can be done in different ways: the oscillating saw, or the single-diameter small bit (or the Shannon strawberry) Which creates orifices in the bone and weakens the bone, creating a succession of orifices in the bone (giving a postage stamp image) retaining a cleverly planned bone bridge that can be supplemented by a manual maneuver.
05
Arthroplasty
Consists in removing one of the two articular surfaces of a joint of a toe such as the interphalangeal articulation, allows to correct the axis and align the toe: grie of a toe.
06
Arthrodesis
Consists of removing the two articular surfaces of a joint of a toe such as the interphalangeal joint, makes it possible to correct the axis and align the toe: grie of a toe, Articulation, by the maintenance of a temporary pin or by the placement of an implant. The disadvantage is that it definitively suppresses the mobility of the joint, it is a therapeutic choice.