or recent rupture, Tendinopathy, Combing, Elongation
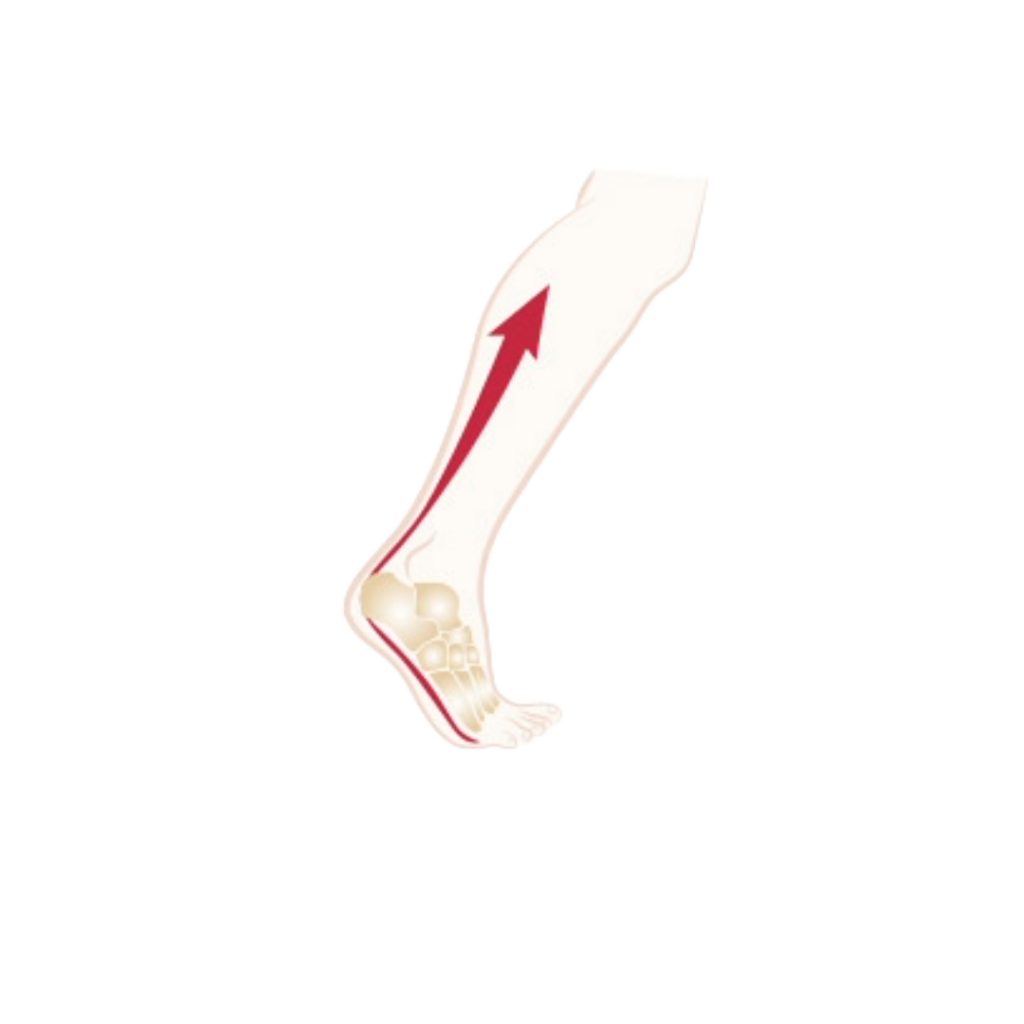
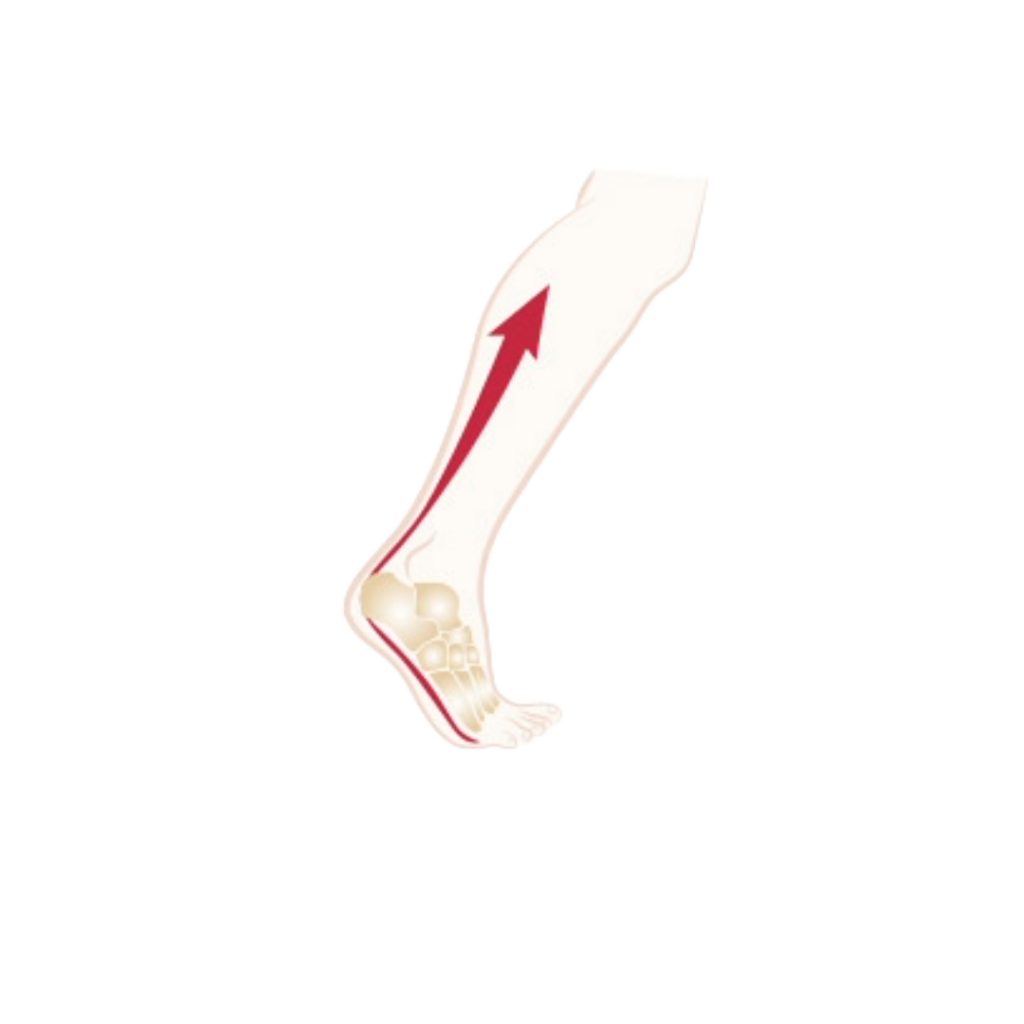
What is the achilles tendon for?
It is the largest and longest tendon in the body. Essential when walking, it has a propelling effect and for this it must be very powerful. Also called the calcaneal tendon, it extends the calf muscle and is inserted on the calcaneum. It “lays” two joints: the knee and the ankle. It unites the tricipital muscle to the heel.
Anatomical reminder
AT (Achille’s Tendon) is ultimately a kind of tendon blade resulting from the union of the aponeuroses of 3 muscles: the 2 twin muscles (2 heads of the gastrocnemius muscle, and the soleus muscle). Flat is a very thick tendon (thickness 5 to 6 mm, 12 to 15 cm long) which ends at the lower part of the posterior surface of the calcaneus on the calcaneal tuberosity. Acting like a powerful lever, it is at the same time fragile and represents a weak point.
Achilles’ tendon :
Q & A
What is a Tendinopathy?
It is an inflammatory pathology of the tendon, which is manifested by tendinitis or peritendinitis. It is a tendency of the tendon, which results in a thickening of the tendon body or tendon sheath and ultimately a histological modification of the tendon tissue itself with the appearance of internal cracks. Clinically, it results in spontaneous (often burning) pain in the heel or on the tendon path during movement and is accompanied by sensitivity to palpation. Without treatment, it can evolve into functional impotence and / or rupture of the tendon.
How do we treat a tendinopathy?
The treatment is primarly medical: The basis of treatment is
- Sports rest,
- Then the plantar flexion of the ankle, in order to shorten the stroke of the tendon, which can be done by a heel, preferably of silicone
- NSAIDs (non-steroidal anti-inflammatory drugs)
- Ice, and Cryotherapy (cold water baths)
- Analgesics (pain relievers), combined with local care (application of ointment, stretching exercises) and a flexible footwear.
And for chronic forms?
Wearing a sole is recommended. This one will try to raise the heel. Shock Waves can, applied by a physiotherapist, break the vicious circle of inflammation and cure or relieve the patient.
What is The “Combing”?
Proposed in forms rebellious to medical treatment, as a therapeutic method, Combing is a simple surgical operation which is done in the open sky by parallel incisions of the tendon body, it can bring thanks to the rest that it imposes; A global healing of the incisions and at the same time it makes it possible to stop or even to cure the inflammation of the tendon. Combing is recommended when pain becomes disabling and when medical treatment becomes inoperative. Several types of intervention can then be proposed.
When is AT Extended?
Congenital retraction (BMI, Little Disease, Equine foot) or acquired (post-traumatic) causes a dorsal flexion deficit of the ankle, or even a vicious equine position of the foot. An elongation becomes indispensable. This can be done transcutaneously or open-air. Followed by plaster immobilisation, or resin, or by an adjustable removable shoe, for a delay of 6 weeks.
Are Infiltrations useful?
If they are done in the peritendineous e zone Or in the “Kräger space” where there is usually an inflammation called retro-calcaneal bursitis, scrupulously avoiding infiltration into the tendinous body itself, they can relieve the patient, break the vicious circle of inflammation and improve the stroke tendon. Some advocate intra tendinous infiltrations, placing the tendon in a discharge and at rest, despite these precautions, the risk of rupture is real. Whatever the seat, infiltrations for TA tendinitis should be avoided because of the high risk of rupture.
1- What is a recent break?
It occurs mostly in athletes (high-level athletes, or recreational sports, with a peak between 30 and 40 years of age) and often on a tendon that is already suffering from an inflammatory, painful and disabling process called tendinitis Achilles. In these cases it is a “fatigue” rupture by an indirect mechanism, a tendon weakened by repeated stress. It occurs more in men.
What is orthopedic treatment for a AT Rupture?
The immobilization, by a plastered boot or in resin, because lighter, or a removable shoe for at least 2 months of which a part in discharge and in equine position (3 weeks at least) Right angle and support, may be indicated, in non-athletes or after 50 years, or diabetic. The results do not include cutaneous necrosis or wound disunion or sepsis, which complicates the outcome of surgical treatment.
2- What if the break is Ancient?
Diagnosis may be delayed and, given the disability that may result, may be a surgical indication, except that the shrinkage of the banks prevents end-to-end implantation. Techniques for grafting or transferring the aponeurosis are then proposed, the best known of which is that of Bosworth.
Is It necessary to operate the AT rupture?
This depends on many factors, but it is possible to proceed surgically:
- Open suturing followed by immobilization: this is a direct suture with a non-absorbable wire end-to-end the edges of the ruptured tendon, followed by immobilization as an orthopedic treatment with the same delay to heal. In a technical variant a lacing of the small plantar is indicated. The disadvantage of surgery is the rate of complication of the skin: local necrosis of the skin, disunion of the wound, bare exposure of the suture, sepsis.
- Or with a closed hearth in percutaneous with synthetic reinforcement: Equine placement, and passage of a reinforcement through the skin of a double lateral and medial reinforcement (Tenolig®), put in tension and left 6 weeks which shelters The tendon the time to heal. The strength of the tendon callus would be of lesser mechanical quality for some authors who report more repetitive ruptures (a second rupture after repair). But if they are carried out by expert hands; The success rate is likely to be higher, which presupposes a period of learning the method of varying length. Especially if the indication is reserved for patients before the age of 50, athletes or very active, without risk factor.
- Or a Mix: Mini-invasive with reinforcement (proposed by the Swiss M. Assal): is a compromise between the two techniques: cutaneous incision (as in b) but only 15 mm to put end to end And suture the tendon followed by the placement of a double reinforcement (as in c). With a strengthened strength and a lower rate of skin complications, this technique seems to be the best solution.
Achilles tendon: Terminology
Tendinopathy: tendon suffering due to intense efforts, leading to an inflammatory process. Also called Tendonitis or peritendinitis.
Combing: A surgical procedure consisting of making incisions parallel to the tendon fibers and putting the tendon to rest to cause it to cicatrize;
Equine: Ankle position of the ankle resting the tendon at rest
Suro-archileo-plantar system: Tendon blade extending from the knee to the heel and ending at the toes
Krager space: triangle between the tendon, upper edge calcaneus and skin
Muscular breakdown: the equivalent of rupture on the insertion of the tendon or the muscular body, sign of the extreme fatigue of the tendon following sudden or repetitive solicitations
Ultrasound: examination confirming the rupture of the tendon or the breakdown, in case of doubt, completed by a more explicit MRI;
Percutaneous suture: surgical method avoiding opening the breaking point, uses a reinforcement placed through the skin and left temporarily.
Reinforcement: Tenolig®: used in closed surgery, associated with immobilization of the tendon can cure it.
Haglund disease: formation of a bony protrusion on the tuberosity of calcaneus, painful (point of friction on the edge of the shoe, can be treated by change of footwear and local care and operated in case of failure or conservative medical treatment
Entemopathy: Rheumatic disease of tendon insertion (SA, FLR, Psoriasis)
Fluoroquinolone: family of antibiotics that weaken and create tendinopathies that can lead to tendon ruptures
Removable Velcro closure with adjustable ankle angle, Walker®, Botimed® or Matrax ™by Donjoy™.